The Road to a Healthy Education May Run Through Medical School
Millions of children in the U.S. have unmet medical needs that make school more difficult. Meet the TFA alumni who are fighting to change that.
When Jerimiah Kouka began his first semester of college at Northeastern University with hopes of one day going to medical school, he arrived with a little more experience than the average high schooler.
Instead of enjoying fun in the sun, Jerimiah spent his last two summers working in labs and shadowing doctors in hospitals around Baltimore—including the renowned Johns Hopkins Hospital, where he did research on the effects of a toxin commonly found in colorectal cancer.
This was all a result of his participation in a program called MERIT Health Leadership Academy. MERIT, which was founded by three Teach For America alumni, is a Baltimore-based nonprofit that educates and empowers students from underrepresented backgrounds to become the next generation of health professionals.
Jerimiah joined MERIT partly because he comes from a family of medical professionals and partly because of the health problems he witnessed in his own community.
Despite being the home of world-class medical institutions like Johns Hopkins, Baltimore has some of the worst health outcomes in the country. The reasons for this are varied and complex, but include generations of poverty, systemic racism, and a lack of diversity in the medical field. Food deserts are common and some neighborhoods are without primary care physicians. Students in the city are at a higher risk of developing conditions like diabetes, asthma, obesity, and lead poisoning, making it harder for them to thrive in school. Jerimiah’s own family struggles with health issues like obesity and diabetes, he says.
“I would see it all my life, but I didn't know what it was. I honestly thought it was the norm,” Jerimiah says. “I didn't know that health disparities meant that different groups are affected disproportionately. Now I understand that this was a systematic oppression built against underrepresented groups."
“It inspired me to be that doctor that would treat their patients beyond the hospital walls, advocate for communities that are less fortunate and actually, holistically treat patients,” he adds.
Today, Jerimiah is working toward his dream of becoming a dermatologist or a family physician. He thinks of one day opening a clinic in an under-represented community like Baltimore, where resources are lacking and there is a great need for preventive medicine.

How Unmet Medical Needs Hold Children Back
It isn’t just Baltimore. Across the country, students are falling behind academically and socially, in part because their medical conditions are being overlooked or untreated. An estimated 4.7 million children in the U.S. have at least one unmet health care need.
Common health barriers to learning include uncontrolled asthma, uncorrected vision problems, uncontrolled diabetes, unaddressed hearing loss, dental problems, persistent hunger, certain untreated mental health and behavioral problems, and the effects of lead exposure, according to research by the healthcare advocacy nonprofit Children’s Health Fund.
These conditions are more prevalent among children in low-income communities and they all do harm to a child’s ability to see and hear in the classroom, focus on classwork, perform on high-stakes tests, and regularly attend school.
There are many reasons for this disparity.
Lack of transportation to see a primary care physician, the sheer scarcity of doctors practicing medicine in low-income communities, financial hardship, and the difficulties of scheduling doctor visits around hourly, shift work all contribute to students not getting the care they need. There is also a historic mistrust of medical professionals within communities of color, particularly among Black communities, as a result of the United State’s troubling legacy of medical research, including the deeply unethical Tuskegee experiment.
Low-income families, with or without insurance, are also more likely to use emergency rooms and less likely to use primary care doctors, even for routine care, according to the Economic Policy Institute.
These are just a few of the many complex causes that lead to low-income students being disproportionately impacted by health issues. Although these students are just as capable of learning as their peers, untreated medical conditions become obstacles that have a devastating impact on a child’s efforts to achieve and thrive in the classroom.
Being a Voice for Her Students
Simran Shah (Miami-Dade 2012) saw these disparities play out in her classroom every day while teaching in the Liberty City neighborhood of Miami.
“Maybe my students aren’t paying attention. Or maybe they have a learning disability, or are behind in their reading level. Or maybe they just can’t see the board, because they've never gotten their vision tested, and they think that’s just what the world looks like,” Simran explains. “It's very hard to differentiate those things without proper intervention, which our schools are not equipped with.”
Simran couldn’t know for sure. And that bothered her.
That's why after three years of teaching through Teach For America, Simran decided to go to University of Miami Miller School of Medicine. “I started to think about how I could still impact my students, but from a different angle,” she explains. “What would be a great niche for me to attack inequity in our population? I thought health was one of the main things.”
While in medical school, she became the project manager for the annual Liberty City Health Fair. She pushed to increase the number of pediatric patients who attend the fair by moving to host the fair at an elementary school in the neighborhood. And she increased the offerings at the pediatric station to include dental and vision. That year, the health fair worked with 67 new pediatric patients—a dramatic increase compared to the fair’s previous average of about three pediatric patients per fair.
It was in medical school when Simran also witnessed prejudice and discrimination from her supervisors and fellow students, and the ways in which this behavior—known as medical bias—shapes a medical system that is often hostile toward children like her students in Liberty City.
“Being in medicine, I’ve worked with a lot of superiors who don’t like serving a certain type of person. They blame diabetes on just the patient,” Simran explains. “I think that being a teacher, and having worked with students intimately, you understand that there’s a reason some students are not eating fruits and vegetables. Working in Liberty City, you know it’s a food desert.”
“And so, when you hear a doctor or fellow medical students make a blanket statement about a Black patient with uncontrolled diabetes who is not taking insulin, saying, ‘Wow, this patient is super non-compliant and they don’t care about their health,’ you get to challenge that with a real-life experience,” she adds.
Simran is currently completing her residency in pediatrics, with intentions to pursue a fellowship in child abuse and neglect. As a passionate advocate for children in the foster system and a guardian ad litem for four young boys, she hopes to focus her future practice on homeless children and children in the foster system.
Pursuing Impact Through Medicine
Seeing students suffer from untreated health conditions without having the resources to help is also what led Annie Dotson, MD (Houston ‘07) to pursue a career in medicine.
“I felt helpless to be able to address these health issues, and I felt they did influence my kids' ability to be present and accountable for,” Annie says. “Even if they really wanted to be, they couldn't be because there were so many other things going on. I felt like, for me, my impact was going to be addressing their health.”

Annie originally aspired to pursue medical school but had put those plans aside to join Teach For America after learning about it from one of her fellow volunteers while she was helping with Hurricane Katrina relief efforts in New Orleans. In the corps, she taught high school science at Lee High School in Houston. But her students refused to let her off the hook for her dreams of becoming a doctor.
“It was actually my students who encouraged me to go onto pursue something medical,” Annie says. “They encouraged me to use my skill set in a way that would still impact their communities, just in a little different way.”
Annie was not the only one in her classroom with that dream. One of her proudest moments from that time was seeing one of her former students get into medical school.
“She sent me a message thanking me for helping her get to that point even though it had been five or six years before,” Annie says. “I just felt so immensely proud of her and all her accomplishments. Actually, on my last count, I have three former students in medical school!”
Today, Annie works as a physician and primary care research fellow at the University of North Carolina at Chapel Hill, where she focuses her research on pregnancy and young children, including the adverse childhood experiences and social determinants of health for children that many of her own students experienced.
Why Representation in Medicine Matters
Both Simran and Annie are determined to advocate for their students’ medical needs in a field that’s not known for its abundance of racial or economic diversity. While people of color make up 26 percent of the total U.S. population, only about six percent of practicing physicians and nine percent of nurses identify as Latinx, Black, or Native, according to Johns Hopkins Medicine. Only one in 20 practicing physicians comes from the poorest 20 percent of families.
The importance of bringing these perspectives into medicine cannot be overstated. At Washington University School of Medicine in St. Louis, the university’s associate dean for diversity, Will Ross, MD, runs a program for first-year medical students that shows them exactly how a neighborhood’s environmental factors—such as green spaces, grocery stores, and public transit lines—directly impact a patient’s health. This helps combat the long-held idea that a patient’s personal choices are the sole reason they are unhealthy, just one example of the impact of bringing more diverse perspectives into medicine as early as medical school.
But even more important for improving medicine is ensuring the children who are impacted by medical disparities today have a chance to solve those problems from within the field itself. That’s the guiding principle behind MERIT.
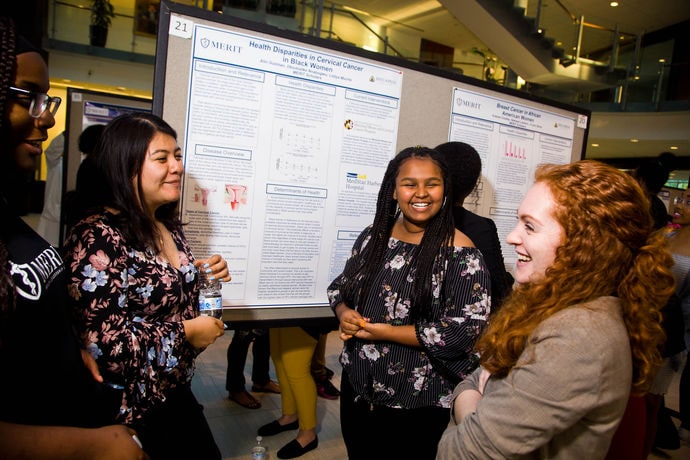
The organization was co-founded in 2010 by Tyler Mains (Baltimore ‘09), Mark Wilcox (Baltimore ’10) and Shyam Gadwal (Baltimore ‘06), all of whom had taught high school science as corps members and saw the difficulties that students with unmet medical needs faced.

One of Tyler’s students, Breonna, suffered from uncontrolled diabetes, causing her to be hospitalized regularly and miss weeks of school because there were no primary care physicians practicing in her neighborhood. Another student, Tyren, aspired to become a doctor and had strong scores in science, yet was underprepared for all hurdles it would take to make it to medical school. MERIT was founded with the goal of empowering students like Tyren to become the doctors of tomorrow who treat patients like Breonna.
That’s because diversity isn’t just a “nice-to-have” in medicine. "It’s a key lever towards reducing health disparities that negatively impact people of color,” says Jake Weinfeld (Baltimore '12), the executive director of MERIT.
“It's really well-documented in the literature that racial concordance between a health provider, like a doctor or nurse, and a patient improves health outcomes,” Jake says.
Lack of representation in medicine also influences the type of medical research being done, which types of patients are centered in a study’s work, and whom the research ultimately benefits. This inevitably impacts health outcomes for entire populations. MERIT seeks to change this for the benefit of all communities like Baltimore. “It’s all about empowering students who've been traditionally underrepresented in the health workforce to become colleges graduate, health professionals, and eventually change agents for Baltimore, and really our entire country,” Jake explains. “We believe that representation is what it's going to take to ultimately create an equitable health care system in our society.”

The Next Generation of Medical Leaders
Since 2010, MERIT has graduated dozens of students like Jerimiah who are driven to lead in medicine and bring the perspectives of their communities into the medical field. The students who make up MERIT’s cohort of scholars have lived experiences that give them first-hand knowledge about the root causes of health disparities.
Through MERIT, they’re given the tools and vocabulary to describe these disparities academically, as well as the opportunities to study them through research fellowships in the country’s top hospitals and labs. But one of the greatest things MERIT provided Jerimiah was the conviction that his lived experiences would be an asset to him as a medical professional. Jerimiah often envisions the patients he wants to treat in the future, and how his upbringing in Baltimore will make him a better and more compassionate doctor.
“Going through similar experiences that patients have gone through, I believe impacts the treatment and research. Coming from an underrepresented community, I will be able to properly relate more once the patient comes in here from a similar community, and not overlook things that are sometimes overlooked,” Jerimiah says. “I can break down the stereotypes about, let's say, someone coming into the hospital. ‘Oh, they're just coming in for just a warm place to lay’ or whatever. That's not the case, actually. People are suffering.”
But for now, Jerimiah is focused on working hard and finishing up his first semester of college at Northeastern University. “It's really surreal when I walk through the quad and I'm in my dorm room and I'm in the study hall,” Jerimiah says. “Honestly, I say this to myself all of the time, ‘I'm living my ancestor's wildest dream.’”
We want your feedback. Share your thoughts on this story or suggest other stories for us to pursue.
Sign up to receive articles like this in your inbox!
Thanks for signing up!
Content is loading...









